Hello everyone! My name is Harshita Gudipudi, and today I will be discussing the effects of socioeconomic status on access to healthcare. While this is a global issue, I will only be focusing on North Carolina in this presentation. I find this topic extremely fascinating because it is not something generally talked about. I myself am an example of this. Like many others, and maybe even yourself, I have never truly witnessed the socioeconomic differences between various social classes as well as how this affects their access to different resources. So, I wanted to address this topic today to educate those who may have also never been exposed to this issue.
So, the main problem is that in today’s society, money equals power. Without money, it is almost impossible to survive. Every necessity must be bought in some manner. Therefore, the higher an individual’s income is, the more opportunities and privileges they will receive. For instance, higher incomes lead to better nutrition, housing, schooling, and recreation (Adler & Newman, 2002, p. 62). Additionally, these individuals have access to healthcare resources such as insurance, medications, and more. This also serves as a reason why one’s socioeconomic status plays such a large role in the quality of their health. According to this chart, socioeconomic factors account for 40% of the social determinants of health, making it one of the largest factors affecting an individual’s overall wellness.
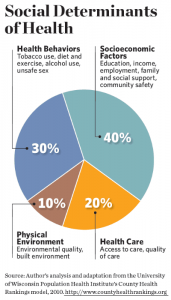
(Mitchell, 2016)
One’s education, income, employment, family, and social support all play a role in their mental and physical health, so without proper medical care, an individual’s health may become detrimental. Therefore, those belonging to lower socioeconomic classes tend to see higher mortality rates, as low socioeconomic status is related to a large range of health issues, such as low birthweight, cardiovascular problems, hypertension, arthritis, diabetes, and cancer (Adler & Newman, 2002, p. 60). Consequently, these individuals tend to have poorer health due to the lack of medical check-ups and treatments.
On the other hand, while socioeconomic status does affect healthcare access, a person’s geographical location also plays a role in the care they receive. Some areas tend to be poorer than others, meaning not as many resources are available there. For instance, in North Carolina specifically, urban areas have a stronger healthcare infrastructure compared to rural areas, which are where individuals of lower economic statuses most frequently tend to live since the cost of living is much cheaper (Holmes, n.d.). These areas are also deliberately less urbanized and developed in order to maintain a natural environment, meaning there are fewer buildings and people present. Therefore, because everything is so isolated, medical facilities are much harder to access and there are fewer medical professionals available. This concept is depicted in this graph.
(Hall & Owings, 2014)
In the graph, there is a significant difference between the percentage values for population and inpatient care in urban areas and rural areas, thus showing the lack of a basic infrastructure in rural places. For instance, the overall population is higher in urban areas, as 83% of them live there while the other 17% live in rural areas. In regards to inpatient care, discharges, days of care, and procedures are all much more prominent in urban areas compared to rural ones (Hall & Owings, 2014). Therefore, the presence of a healthcare infrastructure and access to medical facilities are very strongly correlated with the location the individual resides in.
Now let’s put this concept in the context of North Carolina. In Wake County, there were 23.7 physicians for every 10,000 people in 2010; next door in rural Johnston County, there were only 7.6 (“Down home doctors”, 2016). These statistics, although staggering, depict why it is more difficult to access healthcare in rural areas and why mortality rates are so much higher.
Another reason rural areas have poorer access to healthcare is that the internet services in those areas are far from optimal. Therefore, because these areas are extremely isolated, they are distant from resources such as cell towers and therefore receive inadequate internet service. Additionally, new technology and network services would not be able to solve this problem because wealthier neighborhoods would see these upgrades first (Merschel, 2020). This is evident in this graph, as rural areas have fewer individuals who own certain updated technology such as smartphones, tablets, and laptops.
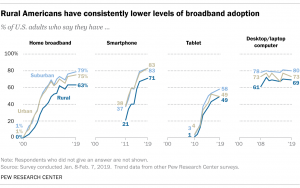
(Perrin, 2019)
As a result, it is much more difficult to complete tasks such as accessing medical records or contacting other medical services, thus minimizing the quality of healthcare. Additionally, telehealth, which is the concept of accessing healthcare services via the internet, would normally solve a multitude of issues such as the lack of medical facilities and professionals in an area, as individuals would be able to contact a healthcare provider with one click of a button. Therefore, the fact that rural areas also have poor internet services reduces the chance of telehealth being the ultimate solution and further facilitates their inaccessibility.
Although this issue encompasses a large part of the world, the effect of socioeconomic status on healthcare can be minimized if individuals decide to take action. One way to minimize this issue is to publicize it because the word could spread to individuals who could make a difference. For instance, a potential donor could hear about it and help establish a more prominent healthcare infrastructure in the areas that lack it. Another way to reduce this issue is to make insurance more affordable because the more people are able to get help with affording healthcare, the more they will be able to get the treatments and medications they require. One more way to minimize this issue is to create partnerships with transportation services because transportation is one of the most daunting hurdles to access care in rural areas (Cheney, 2018). By providing free transportation services, more people would be able to travel to an area that has a better medical system.
To sum up, one’s socioeconomic status plays a key role in their life. Money and social class essentially determine what opportunities people can receive; they are prominent factors in all our lives. Without a solid income, we would not be able to receive a good education, a nutritional diet, a secure place to live, or any luxuries. However, an individual’s income should not have to determine their quality of health, which is why healthcare should be accessible no matter what socioeconomic class one is a part of. We have the ability to educate the world and attempt to reduce mortality rates everywhere, so why not take advantage of it?
Thank you for your time.
References
Adler, N. E., & Newman, K. (2002). Socioeconomic disparities in health: Pathways and policies. Health Affairs, 21(2). 60-76. doi:https://doi.org/10.1377/hlthaff.21.2.60.
Cheney, C. (2018, September 21). 3 ways providers can improve healthcare access in rural areas. HealthLeaders Media. https://www.healthleadersmedia.com/clinical-care/3-ways-providers-can-improve-healthcare-access-rural-areas.
Down home doctors: Poor access to healthcare in rural NC. (2016, June 3). NC Coalition for Fiscal Health, https://www.fiscalhealthnc.com/down_home_doctors_poor_access_to_healthcare_in_rural_nc.
Hall, M. J., & Owings, M. (2014, November). Rural and urban hospitals’ role in providing inpatient care, 2010. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/products/databriefs/db147.htm.
Holmes, M. (n.d.). Access to healthcare in rural North Carolina. North Carolina General Assembly, https://www.ncleg.gov/documentsites/committees/bcci-6715/January%208,%202018/3.%20Holmes,%20Rural%20Healthcare%20by%20the%20Numbers.pdf.
Merschel, M. (2020, August 5). High-speed internet offers key connection to health, but millions lack it. American Heart Association. https://www.heart.org/en/news/2020/08/05/high-speed-internet-offers-key-connection-to-health-but-millions-lack-it.
Mitchell, F. (2016). Innovations in health equity and health philanthropy . Stanford Social Innovation Review: Informing and Inspiring Leaders of Social Change. https://ssir.org/articles/entry/innovations_in_health_equity_and_health_philanthropy#.
Perrin, A. (2019, May 31). Digital gap between rural and nonrural America persists. Pew Research Center. https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/.
Featured Image Source:
Google Images, Creative Commons license.